The concept of ovarian reserve plays a pivotal role in a woman’s reproductive health, influencing her fertility and overall well-being. Understanding the intricacies of ovarian reserve is crucial for individuals contemplating family planning or seeking fertility treatments. In this comprehensive guide, we delve into the various facets of ovarian reserve, shedding light on its definition, factors affecting it, and the available testing methods.
Defining Ovarian Reserve
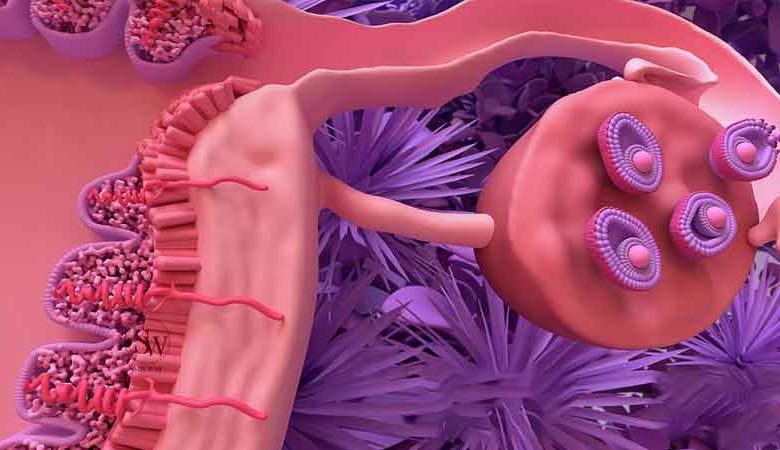
Ovarian reserve refers to the quantity and quality of a woman’s eggs, also known as oocytes, in her ovaries. This reservoir of eggs represents a key determinant of fertility, as it reflects the reproductive potential of an individual. The ovarian reserve is finite and gradually declines with age, impacting a woman’s ability to conceive naturally.
Factors Affecting Ovarian Reserve
- Age: The most significant factor influencing ovarian reserve is age. As women age, the number and quality of eggs diminish. This decline accelerates after the age of 35, making it more challenging to conceive.
- Genetics: Genetic factors can also contribute to variations in ovarian reserve. Some women may have a genetic predisposition to experience a more rapid decline in ovarian reserve compared to others.
- Lifestyle Factors: Certain lifestyle choices, such as smoking and excessive alcohol consumption, can negatively impact ovarian reserve. Maintaining a healthy lifestyle, including regular exercise and a balanced diet, is essential for preserving ovarian health.
- Medical Treatments: Certain medical treatments, such as chemotherapy or pelvic surgeries, can have a detrimental effect on ovarian reserve. It is crucial for individuals undergoing such treatments to discuss fertility preservation options with their healthcare providers.
Ovarian Reserve Testing Methods

- Anti-Müllerian Hormone (AMH) Test: The AMH test measures the level of a hormone produced by ovarian follicles. A higher AMH level indicates a larger ovarian reserve. This blood test is commonly used to assess fertility potential.
- Follicle-Stimulating Hormone (FSH) Test: FSH is a hormone released by the pituitary gland, and elevated levels can indicate a diminished ovarian reserve. FSH testing is often performed on specific days of the menstrual cycle to evaluate ovarian function.
- Antral Follicle Count (AFC): This ultrasound-based test assesses the number of small follicles in the ovaries. A lower AFC may suggest a reduced ovarian reserve.
- Ovarian Volume Measurement: Measuring the volume of the ovaries through ultrasound can provide additional insights into ovarian health.
Fertility Preservation and Enhancement:
For individuals concerned about their ovarian reserve, there are proactive measures that can be taken to preserve fertility:

- Egg Freezing: Women can opt for egg freezing (oocyte cryopreservation) to preserve their eggs at a younger age, ensuring a higher likelihood of successful conception later in life.
- Healthy Lifestyle Choices: Adopting a healthy lifestyle, including maintaining a normal BMI, avoiding smoking, and limiting alcohol intake, can positively impact ovarian reserve.
- Timely Family Planning: Understanding one’s ovarian reserve can inform family planning decisions. Seeking fertility consultation at an earlier age can facilitate informed choices.
What is a Normal Ovarian Reserve Count?
The term “normal” ovarian reserve count refers to the average number of viable eggs a woman has in her ovaries, considering her age. While there isn’t a universal standard for normal ovarian reserve, healthcare professionals often use certain tests to assess the quantity and quality of eggs, such as the Anti-Müllerian Hormone (AMH) test, follicle-stimulating hormone (FSH) test, and antral follicle count (AFC) through ultrasound. Generally, a higher ovarian reserve count is associated with better fertility potential.
What is a Good AMH Level for Each Age?
| Age Group | Optimal AMH Level (ng/mL) |
|---|---|
| 20-24 | 2.0 – 6.8 |
| 25-29 | 1.8 – 6.8 |
| 30-34 | 1.4 – 6.7 |
| 35-39 | 0.9 – 5.4 |
| 40-44 | 0.2 – 4.1 |
| 45+ | 0.1 – 2.2 |
These values are general guidelines, and individual variations may exist. It’s essential to interpret AMH levels in conjunction with other factors and consult with a healthcare professional for personalized advice.
Can I Get Pregnant with a Low Ovarian Reserve?

While a low ovarian reserve may decrease the chances of conceiving naturally, pregnancy is still possible. Assisted reproductive technologies, such as in vitro fertilization (IVF), may be recommended to enhance the chances of conception. Consulting with a fertility specialist can provide tailored guidance based on individual circumstances.
Low Ovarian Reserve Symptoms
Identifying symptoms of low ovarian reserve can be challenging as it often manifests silently. However, women with low ovarian reserve may experience irregular menstrual cycles, difficulty in conceiving, or an earlier onset of menopausal symptoms. Consulting with a healthcare provider is crucial for accurate diagnosis and guidance.
How to Improve Ovarian Reserve?
While the natural decline in ovarian reserve is unavoidable, certain lifestyle choices can positively impact ovarian health:
- Maintain a Healthy Lifestyle: Adopt a balanced diet, regular exercise, and avoid smoking or excessive alcohol consumption.
- Consider Fertility Preservation: If family planning is postponed, consider options like egg freezing to preserve eggs at a younger age.
- Early Family Planning: Understanding ovarian reserve early can inform family planning decisions, allowing for timely fertility interventions if needed.
- Consult with a Healthcare Professional: Regular consultations with a healthcare provider specializing in reproductive health can provide personalized guidance and support.
Does Low Ovarian Reserve Mean Early Menopause?

While low ovarian reserve and early menopause share a connection in terms of declining reproductive capacity, they are not synonymous. Low ovarian reserve implies a diminished quantity and quality of eggs in the ovaries, potentially impacting fertility. Early menopause, on the other hand, refers to the cessation of menstrual cycles before the age of 40. While low ovarian reserve can be a factor contributing to early menopause, they are distinct concepts.
What Causes Diminished Ovarian Reserve?
Diminished ovarian reserve can result from various factors, and it is often a complex interplay of genetics, lifestyle, and medical history. Some key contributors include:
- Age: The most common cause of diminished ovarian reserve is advancing age. As a woman gets older, the quantity and quality of eggs naturally decline.
- Genetic Factors: Genetic influences can contribute to variations in ovarian reserve. Some individuals may have a genetic predisposition to experience a more rapid decline.
- Autoimmune Disorders: Certain autoimmune conditions, such as autoimmune ovarian insufficiency, can impact ovarian function and contribute to diminished ovarian reserve.
- Chemotherapy and Radiation: Medical treatments like chemotherapy and pelvic radiation can have detrimental effects on ovarian health, leading to a decline in ovarian reserve.
- Ovarian Surgeries: Surgical procedures involving the ovaries, especially those that remove ovarian tissue, can reduce the overall ovarian reserve.
- Smoking and Excessive Alcohol Consumption: Unhealthy lifestyle choices, such as smoking and excessive alcohol intake, are associated with a faster decline in ovarian reserve.
- Endometriosis: Endometriosis, a condition where tissue similar to the lining of the uterus grows outside the uterus, can negatively impact ovarian function and lead to diminished ovarian reserve.
- Previous Ovarian Cysts: Ovarian cysts, especially those requiring surgical intervention, may affect the ovarian reserve.
FAQs:
- Can ovarian reserve be improved?
While certain lifestyle changes may positively influence ovarian health, the natural decline in ovarian reserve with age is inevitable. Proactive measures such as maintaining a healthy lifestyle and considering fertility preservation options can, however, contribute to better reproductive outcomes. - Is there a specific age to start testing ovarian reserve?
Ovarian reserve testing is often recommended for women in their late 20s to early 30s, as it provides valuable insights into fertility potential. However, individual circumstances may vary, and consultation with a healthcare provider is essential. - Are there alternative methods for fertility preservation besides egg freezing?
Yes, besides egg freezing, other fertility preservation methods include embryo freezing and ovarian tissue freezing. The choice of method depends on individual circumstances and preferences. - Can medical treatments impact ovarian reserve permanently?
Some medical treatments, such as certain chemotherapy regimens, can have a lasting impact on ovarian reserve. It is crucial for individuals undergoing such treatments to discuss fertility preservation options with their healthcare providers before starting treatment.
Conclusion
Understanding and addressing ovarian reserve is pivotal for women navigating their reproductive journey. By comprehending the factors influencing ovarian reserve, undergoing timely testing, and considering proactive measures, individuals can make informed decisions to enhance their fertility potential. As fertility awareness continues to grow, empowering women with knowledge about ovarian reserve becomes increasingly crucial in promoting reproductive health and family planning.



